Dentistry affords the unique opportunity to blend both art and science. I enjoy the artistry of creating beautiful smiles and caring for each patient individually. But, I also get to exercise my passion for science, constantly reading and studying in an effort to provide the best treatment and advice for home care. Sometimes, new information becomes available and as scientists we are challenged to embrace the latest research instead of taking the easy path of doing as we've always done.
Prosthetic Knees & Hips
About a decade ago, the clinical practice guidelines for patients with prosthetic joint replacements (knee and hip replacements) made a major shift. NO LONGER are patients recommended to take an antibiotic before dental treatment. My approach to this change had been somewhat lax due to the pressure felt to cling onto an old habit. It was especially difficult to go against the majority of orthopedists still encouraging their patients to follow the outdated guidelines. But, years worth of research have provided evidence that this practice is an all risk/no benefit for the majority with an artificial knee or hip joint.
You may wonder why having a dental procedure could be connected to an infection of a knee or hip joint. A dental procedure, flossing or brushing your teeth and chewing food are all possible scenarios that could cause the gum tissues to be cut/lacerated and bacteria from the oral cavity could enter your bloodstream. This could cause something known as a bacteremia, an invasion of bacteria into your bloodstream. These bacteria have the ability to travel through your circulatory system and could infect prosthetic joints.
Old Habits Die Hard
In 2012, the American Academy of Orthopedic Surgeons and the American Dental Association published a report of evidence based clinical guidance to make the recommendation that 'the practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures'.
In 2014, a panel of experts convened to clarify the 2012 report and included 4 case controlled studies. The conclusions were:
In general, for patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection. The practitioner and patient should consider possible clinical circumstances that may suggest the presence of a significant medical risk in providing dental care without antibiotic prophylaxis, as well as the known risks of frequent or widespread antibiotic use. As part of the evidence-based approach to care, this clinical recommendation should be integrated with the practitioner’s professional judgment and the patient’s needs and preferences.
Said more simply, most patients with a hip or knee replacement SHOULD NOT be taking antibiotics prior to dental treatment. Outlying cases do exist and they should be considered on an individual basis.
We are now a decade beyond when this was published and to date there are NO STUDIES that support the benefit of taking an antibiotic prior to dental procedure and yet almost every patient is still given this recommendation from their orthopedic provider. Why? Are they unaware of the current Clinical Practice Guidelines? Are we prescribing to just feel like we're doing something? I don't know the answers but my position had been to just default to what the orthopedic surgeon recommended. But, based on the current evidence of the risks associated with unnecessary antibiotic prophylaxis, I can no longer support this outdated practice. Here are some statements/research to consider:
Case control study with 339 patients with joint replacement and prosthetic joint infection and 339 matched controls with NO infection
NO ASSOCIATION between having undergone high risk dental procedure without antibiotics and a joint infection at 6 months or 2 years
taking an antibiotic DID NOT decrease likelihood of joint infection
Risk of infection increases with INCREASING comorbidities: obesity, rheumatoid arthritis and immunosuppressive medications
Conclusion: "We believe that reported PJIs attributed to dental procedures are more likely to have been caused by bacteremia related to routine daily activities than by bacteremia related to dental procedures. It is INCONSISTENT to recommend prophylaxis of prosthetic hip or knee infection for dental procedures but not to recommend prophylaxis for these same patients during routine daily activities."
Joint statement with Canadian Orthopedic Assoc and Association of Medical Microbiology and Infectious Disease
Patients should NOT be exposed to the adverse effects of antibiotics when there is NO EVIDENCE that such prophylaxis is of any benefit
Patients should be in optimal oral health prior to joint replacement
No significant positive association was identified between IDPs and LPJI.
These results should reassure orthopedic surgeons and their patients that dental care of patients who have prosthetic joints should focus on maintaining good oral hygiene rather than on recommending AP for IDPs. Moreover, it should also reassure those in other countries where AP is not recommended that such guidance is sufficient.
The Risk
You may wonder, what's the big deal?? Why not just take an antibiotic to feel 'safe'??
Antibiotic risks:
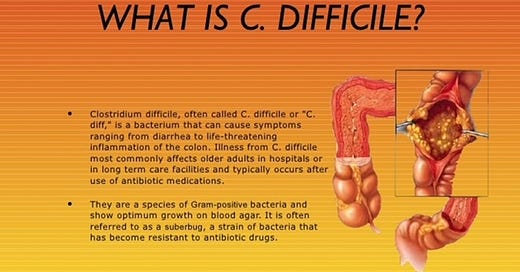
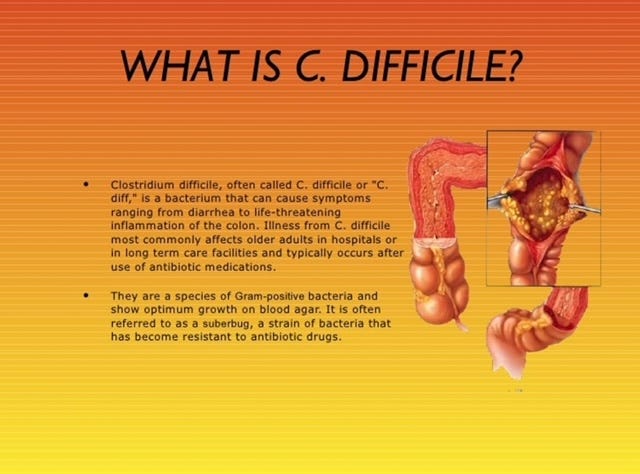
Overuse of antibiotics increases the likelihood of resistant organisms
35,000 deaths/yr due to antibiotic resistance
increased risk for C. difficile infection which is known to cause about 29,000 deaths/year
Unfortunately, the belief that dental procedures somehow increase the risk of joint infection is unfounded and has likely instilled an unnecessary level of fear about dental cleanings. A 2016 study, amongst others, has demonstrated the opposite is actually the case, frequent and regular dental scaling is associated with a reduced risk of prosthetic joint infections in total knee replacement patients.
If you are a patient with a prosthetic joint and your provider insists that you take an antibiotic prior to dental procedure, I would urge you to ask why he or she is making a recommendation that goes against all available evidence. There are certain to be cases of increased risk that deserve to be discussed with both the patient and the dental provider. I would encourage you to ask for this evidence and ultimately make the best risk assessment for yourself.
Photo of a patient’s dog who likes to show off his beautiful smile 😊. I hope his smile brightens your day!!



I wish all dentists were like you! Most just stick with what they were taught, even though there could be more recent studies that question their beliefs or ways of doing things. Great job, Dr. Funk! We learn so much from you! Thank you!
Can’t say I know anything about that. That said, the worst illness I have ever suffered from was when a dentist gave me a filling that got infected. I felt like I was on death’s door and it was the root canal dude who sorted me out, with a special kind of anti biotic after the normal ones didn’t work. I was quite surprised that such a little “wound” decked me out with fevers etc. I guess modern surgery wouldn’t be possible without them.